Cervical Mri Bright Spot at Back of Skull
Cover Story: Revealing the Mysteries behind Magnetic Resonance Imaging
by Jill Conway, MD, MA, MSCE
Reviewed by Jack Burks, MD
Edited by Susan Wells Courtney
Introduction
When someone presents with a symptom typical of multiple sclerosis (MS), such as optic neuritis, vertigo, or numbness and tingling, a clinician often orders magnetic resonance imaging (MRI). This technology reveals the inside of the brain, eye, and spinal cord in a painless, noninvasive method. The brain and spinal cord make up the central nervous system (CNS). While X-rays and computed tomography (CT) scans provide some detail about bones and some body tissues, an MRI reveals much more detail about tissue in the CNS, showing both the normal structure of the brain and spinal cord, as well as the presence of lesions, scars, or tumors.
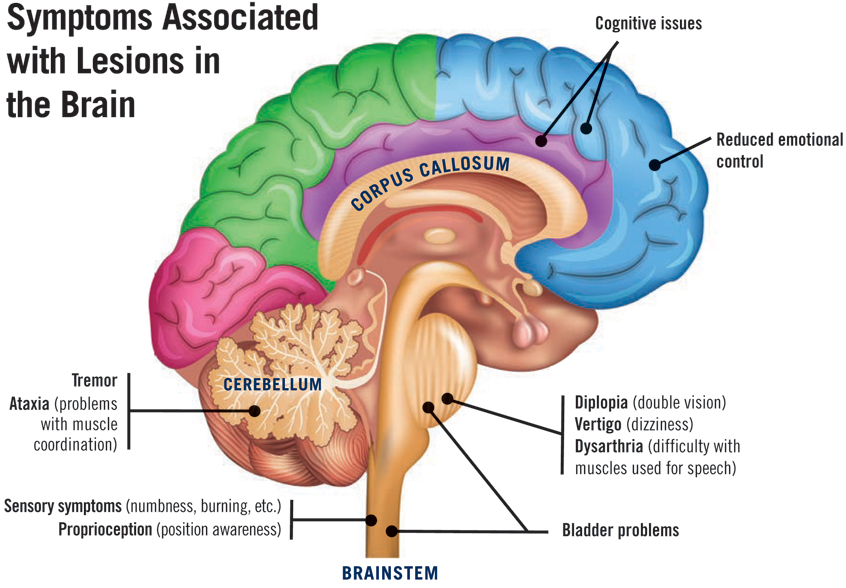
 When MS causes a specific symptom – vertigo, loss of vision, or numbness for example – sometimes a lesion can be seen on an MRI in a region of the brain that correlates to the symptom. A lesion is an area of inflammation or damage within the CNS. Finding such lesions helps with the diagnosis of multiple sclerosis and assists with ruling out other possible conditions, such as a tumor or stroke.
When MS causes a specific symptom – vertigo, loss of vision, or numbness for example – sometimes a lesion can be seen on an MRI in a region of the brain that correlates to the symptom. A lesion is an area of inflammation or damage within the CNS. Finding such lesions helps with the diagnosis of multiple sclerosis and assists with ruling out other possible conditions, such as a tumor or stroke.
In addition to diagnosis, the MRI aids prognosis (predicting the likely course of one's disease) and disease management in multiple sclerosis. The number of lesions on an MRI, their location, and their size can predict disease severity, even early in the course of MS. The overall burden of disease at diagnosis and the location of lesions impact treatment choices and whether the risks of a specific treatment outweigh the benefits.
Once someone with MS starts a disease-modifying therapy (DMT), a periodic MRI assesses whether the treatment is working. If new lesions are detected after starting a therapy, then an MRI demonstrates that the individual may not be responding well to the treatment and a change may be considered. An MRI thus helps with diagnosis, prognosis, and monitoring the response to an MS treatment.
MRI can be useful when someone has an MS exacerbation – also known as a relapse or flare-up. With a relapse, an individual experiences new or worsening symptoms of MS. During relapses, the treating physician may order MRI to evaluate whether new inflammation is occurring in the brain or spinal cord.
Despite these advantages, an MRI poses challenges for individuals with MS. Many people feel claustrophobic in the small MRI tube and this makes it difficult for them to lie quietly for the length of an MRI, which can last up to an hour for multiple scans. Cost provides another barrier to obtaining an MRI, as many either do not have insurance or face an expensive co-pay. Sometimes insurance carriers will deny coverage of an MRI, even for individuals with MS where this monitoring is a standard of care.
This article presents an overview of MRI for individuals with MS – how MRI works, what it shows, how MRI techniques and machines differ, and challenges to getting an MRI. This article also explains how MRIs are used for monitoring disease activity and for evaluating treatment response. We hope to help reveal the mysteries behind magnetic resonance imaging, ultimately enabling members of the MS community to better understand why they are having an MRI and what the specific results will mean for them.
What is an MRI and How Does it Work?
 As noted earlier, MRI stands for "magnetic resonance imaging." Because images are obtained by a magnetic field, no harmful radiation exposure occurs with an MRI scan. Provided that the patient has no metal on or embedded in his or her body, exposure to an MRI is safe.
As noted earlier, MRI stands for "magnetic resonance imaging." Because images are obtained by a magnetic field, no harmful radiation exposure occurs with an MRI scan. Provided that the patient has no metal on or embedded in his or her body, exposure to an MRI is safe.
Read more on the safety of using contrast dyes.
Generally, when the body's tissues are exposed to a magnet, the protons (hydrogen atoms most commonly found in water) in the tissues orient themselves in the direction of the field, similar to how a compass needle lines up with the earth's magnetic field. Turning the magnetic field on and off makes the protons line up and relax repeatedly, which releases energy that can be measured by a receiver in the MRI machine. Different tissues have varying amounts of protons, and thus, bone, fluid, and brain tissue all send different signals to the receiver. Computer software converts the received signals into a map of the tissue – based on the water content and response to the magnetic field.
As a person lies in the MRI tube, this process creates different pictures through different planes of the tissue being examined. These are different positions from which the computer takes its images. Some images will show the tissue in a cross-section, called an axial plane. Some images will show the tissue in slices from right to left, called a sagittal image, and others will show front-to-back images, called coronal sections.
What Does an MRI Show?
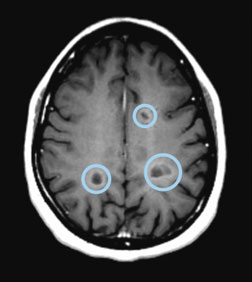
Axial T1 image of the brain showing black holes (circled)
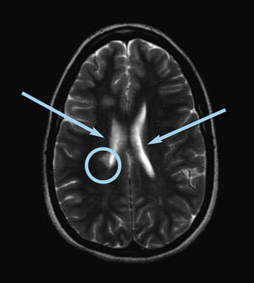
Axial T2 image of the brain showing a lesion as white (circled) and fluid as white (see arrows)
The MRI uses different pulsing techniques to create different images. The images that are created by each separate pulsing are called sequences. Each sequence of pulses has a different sound heard by the person lying in the tube.
T1, T2, FLAIR, and T1 with gadolinium refer to different MRI sequences. These different pulse sequences each show the fluid and tissue differently on the brain and spinal cord images. Certain features and changes in the tissue appear more prominently, depending on the type of sequence used.
A normal brain has gray matter around the outside and white matter deeper in the brain. The gray matter contains the brain cells or neurons that generate impulses and thoughts. The white matter helps conduct the impulses generated to other parts of the brain or to the spinal cord, usually through axons (the nerve fibers of the CNS) surrounded by myelin (the protective covering). T1 imaging preserves this relationship in the images produced – the gray matter is darker than the white matter. T1 imaging shows normal structure extremely well, but seeing lesions on this kind of imaging can be difficult.
One kind of lesion that can be seen best on T1 images is a black hole. When an MS lesion forms and heals over time, sometimes the myelin partially repairs itself and the underlying structure remains. Other times, however, damaged axons and neurons cannot be repaired and brain tissue is lost. This process forms a black hole. A chronic black hole, present for more than six months, indicates the permanent loss of tissue. Black holes can be associated with more cognitive dysfunction and disability. Fortunately, some MS medications reduce the number of new lesions formed in MS, which can reduce the formation of black holes.
T2 imaging reverses the color of gray and white matter on MRI images. White matter looks darker and gray matter looks lighter. This sequence displays lesions as bright white spots or scars on the images. However, with T2 imaging, the cerebrospinal fluid, which is the normal fluid in and around the brain and spinal cord, also appears bright white. Seeing white spots next to an area of bright white fluid can be difficult. So although T2 imaging shows pathology or abnormal tissue well, it is limited by the confusion between the fluid and the spots.
FLAIR images resolve this difficulty. FLAIR stands for fluid attenuated inversion recovery, which basically means that the bright fluid on T2 imaging gets converted into black in the image. Thus FLAIR images show lesions as bright white spots and fluid as dark black; this helps make the lesions clearer and easier to see. On FLAIR and T2 images, old lesions and new lesions can be seen. Lesions are visible as they arise during the stage of acute inflammation, but they also tend to stay for many years afterward as a scar. Rarely, lesions will heal so well that they can no longer be seen on T2 or FLAIR images, but the majority will be visible on future MRIs.
MRI with Contrast
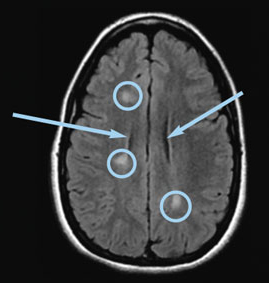
Axial FLAIR image of the brain showing lesions as white (circled) and fluid as black (see arrows)
Often an MRI will be done with contrast. What does this mean? In a sequence with contrast, T1 images are created after a contrast dye has been injected into the patient's vein. Once contrast is given, it travels through the bloodstream and into the blood vessels in the brain and spinal cord.
These vessels can be seen clearly on an MRI after the contrast has been injected. If active inflammation in the brain or spinal cord with a lesion is currently taking place at the time of the MRI, the blood vessels near the lesion will be "leaky." This happens as part of the body's basic response to injury and inflammation. Blood vessels become leaky so that white blood cells and other responses to injury can get into the damaged tissue.
In the brain and spinal cord with MS, a new lesion forming will have leaky local blood vessels. When the contrast dye is introduced, the dye leaks out and the area near the lesion shows up very brightly on this kind of image. These lesions are called "enhanced," "bright with contrast," or "active" on typical MRI reports.
Enhancing lesions have important meaning for clinicians as they indicate current disease not being adequately controlled by an MS treatment. A newly formed lesion usually enhances for a few weeks before blood vessels seal again and the blood-brain barrier (BBB) is restored. The BBB is a protective barrier that lines the blood vessels, designed to prevent damaging cells and other substances in the blood from entering the CNS. See additional details on the safety of using contrast dyes.
How MRI Machines Differ
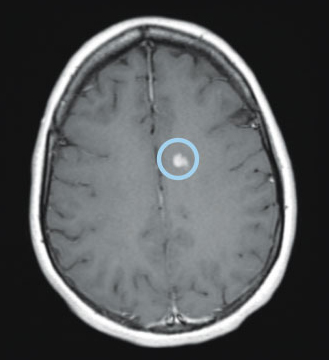
Axial T1 image with gadolinium of the brain showing an enhancing lesion (circled)
Different MRI machines produce images of varying quality, partly depending on the strength of the magnet used, which is measured in teslas. Higher teslas indicate greater magnet strength. Many commercial MRIs use 3.0 tesla magnets, although 1.5 tesla magnets are frequently used as well. Magnets with a strength greater than 3.0 tesla can be used in research trials. Regardless of the specific tesla strength, because all MRIs use powerful magnets, having metal in the body or on the body as jewelry when having an MRI can be dangerous.
Open MRIs use lower tesla magnets (usually 0.3 to 0.7 tesla) and obtain lower-resolution images than traditional MRIs (at 1.5 and 3.0 tesla). For comparison, an average refrigerator magnet would have about 0.001 tesla strength. An open MRI, as the name implies, allows more open space around the individual, with the equipment above and to the side of the patient. Think of these lower-resolution images as being similar to having fewer pixels on a camera image, on a computer monitor, or on a TV screen. With fewer pixels, fewer details can be seen.
While valuable for those with severe claustrophobia (a fear of tight spaces), open MRIs create images with less clarity. For some purposes, such as seeing larger lesions in the brain hemispheres, reduced clarity works. For others, such as looking at tiny lesions in the spinal cord or optic nerve, higher resolution is needed to improve the accuracy and usefulness of the images.
COMPARING TESLA STRENGTHS | |
| Refrigerator | .001 |
| Open MRIs | 0.3 to 0.7 |
| Traditional MRIs | 1.5 and 3.0 |
| MRIs for Research | 7.0 or more |
Other options are available, including those with normal strength (1.5 and 3.0 tesla), but without the traditional "closed-bore" tube. Some facilities now offer MRIs with either a "wide-bore" or "short-bore" design, which can help to fit larger patients (up to 500 pounds in some cases), and can help individuals to feel less claustrophobic. Some MRIs allow for a person to be in a seated position, which can help those who have trouble lying down for an MRI.
A clinician orders an MRI with specific instructions, including the body part to be examined, specific additional sequences desired, and the use of contrast, if needed. Many MRIs are ordered with and without contrast, which means that the images are taken before contrast, and then T1 images are retaken after the patient has contrast injected.
When ordering MRIs, each specific part of the body will need a separate MRI. If the concern is for optic neuritis, a separate MRI of the eye and orbit around the eye may be ordered. If symptoms are present that may indicate spinal-cord disease, the spinal cord may be included with the neck (cervical spine), or the spinal cord in the torso (thoracic spine). If someone has an acute symptom indicating potential relapse, contrast will usually be given to assess whether active inflammation is currently taking place.
The Importance of Age, Context, and Location of Lesions
The brain MRI of a young and healthy person should not have any lesions, spots, or plaques (scarred areas) visible on an MRI. The interior of the brain seen on an MRI appears symmetric. The brain appears to fill up the space inside the skull as no brain atrophy is present.
When an individual presents with a symptom typical of MS, the initial brain MRI helps to establish a diagnosis. As noted earlier, although some MS lesions heal so well that they are no longer visible on an MRI, most MS lesions remain present as "sclerosis" (which refers to hardening or scarring), and this can be seen even years later.
Not all lesions or spots indicate MS. As we age, the brain also ages. Bright spots on an MRI can develop due to conditions other than MS – including stroke, head trauma, migraine headache, or Vitamin B12 deficiency.
Certain infections, or other autoimmune diseases such as lupus or sarcoidosis, are associated with increased lesions in the brain. Cigarette smoking, diabetes, high cholesterol, and high blood pressure cause damage to the small blood vessels in the brain, which can also lead to bright spots on MRI.
To diagnose MS with an MRI, context matters. A healthy 17-year-old brain should have fewer scars than an 80-year-old with a history of smoking and diabetes. If the 17-year-old presents with blurry vision typical of optic neuritis and lesions in the brain, MS may be likely. In an 80-year-old person, brain changes may reflect aging and the probability of the scars being MS would be less likely.
The location of the lesions also matters for diagnosis. While lesions associated with multiple sclerosis can appear anywhere in the brain or spinal cord, they occur more frequently in specific locations, such as near the corpus callosum (a bundle of fibers connecting the two hemispheres of the brain), perpendicular to the fluid-filled ventricles, or in the brainstem.
Multiple sclerosis lesions arise from the white matter, with fewer lesions seen in the gray matter on commercial MRIs (those with standard tesla strength of 3.0 or below). This is in contrast to the MRIs used for research, which have stronger magnets and can more easily show lesions in the gray matter.
Lesion shape and size assist with diagnosis. MS lesions tend to be oval shaped and about a centimeter in diameter. Bright spots or lesions are commonly present in an aging brain, but spinal cord changes are rare. Spinal cord lesions typically indicate disease, although not necessarily MS.
Let's imagine someone visiting a clinician, and he or she reports double vision when looking to the right. This is a classic symptom of multiple sclerosis, but it can also result from other conditions such as a stroke or tumor. The clinician orders an MRI to evaluate the symptom. The MRI may show a brainstem lesion that enhances with contrast, demonstrating that the lesion developed recently – over the last few weeks – and likely caused the symptom.
Multiple sclerosis, however, implies that "multiple" lesions are present, and these occur over time. If the MRI shows many other scars, including older lesions that are not active, it demonstrates that the disease process is ongoing and not a single, isolated event. If these lesions exist in locations typical of MS – near the ventricles or in the spinal cord – and the person tests negative for other conditions associated with such lesions (these conditions are sometimes referred to as "MS mimickers"), then MS becomes a likely diagnosis, provided imaging features do not demonstrate signs of a stroke or tumor.
To summarize, at the time of diagnosis, the MRI helps with prognosis. Research suggests that individuals with more lesions on the initial MRI may have a more severe disease course. Lesions in the spinal cord are worrisome as those who have many spinal cord lesions tend to have worse disability in the future. The presence of brain atrophy and black holes predicts increased disease progression over time. Early recognition and effective treatment of MS lessens the chance of disease progression.
Using MRI in Disease Management
Although this surprises some individuals with MS, many MRI lesions in the brain are clinically silent, meaning that they cause no symptoms at all. A lesion in the optic nerve may lead to decreased vision, but small lesions in the brain rarely cause a symptom. For this reason, clinicians order surveillance MRIs to assess whether new lesions are present, even if no new symptoms have occurred. These surveillance MRIs help establish whether a medication for MS is working adequately. After a certain amount of time has passed, if someone has new lesions while on medication, the clinician may consider whether another disease-modifying therapy (DMT) may provide better protection from breakthrough disease (this refers to continued disease activity despite treatment).
Evaluating breakthrough disease can be tricky, as it depends on timing. Most DMTs work within a few months of starting treatment, but not instantly. If someone has an MRI in January, leading to diagnosis in February, therapy may not begin until March or April, after all testing and insurance approvals are complete. If the therapy requires six months to reach its full effect, an MRI done in June may show active disease not yet suppressed by the DMT.
Concluding that a medication does not work when it hasn't had enough time to take full effect would certainly be an unfair assessment. However, an MRI done six months after starting the DMT, in October for the example above, gives adequate time to suppress new disease activity. For this reason, clinicians commonly order MRI six-to-twelve months after beginning a new disease-modifying therapy. This MRI should not show any active or enhancing lesions, as ideally the DMT should prevent active disease.
When starting a new DMT, new lesions might appear before the new medication takes effect. Thus, the six-month MRI may show additional lesions not seen at diagnosis. These lesions likely occurred before the full benefit of therapy and do not necessarily indicate treatment failure. An MRI six-to-twelve months after starting a medication establishes a new baseline on therapy. Since the therapy should now be effective, future MRIs will hopefully show no changes from this new baseline.
Repeat imaging at the same imaging center should allow a radiologist to compare between MRIs and note any changes in the time between scans. Guidelines recommend repeating a brain MRI every year or two to assess for silent disease activity or progression of atrophy. For someone on the same therapy for many years whose disease activity is stable, less frequent imaging (every two-to-three years) may be adequate.
If someone is taking a DMT that increases the risk of certain infections such as progressive multifocal leukoencephalopathy (PML), annual imaging should be considered. PML is a potentially fatal brain infection that can occur in people with a weakened immune system, which can result from taking an immunosuppressant. For specifics on the latest MRI recommendations, please see CMSC's Proposed 2018 Revised MRI Guidelines.
Because MS can affect the entire central nervous system, initial MRIs may include the brain, cervical spine (neck), and thoracic spine (torso). These images help with choosing a DMT and illustrate the initial burden of disease and disease severity at onset. Subsequently, many clinicians order brain MRIs at regular intervals, but assess the spinal cord less frequently because fewer clinically silent lesions occur in the spinal cord. In addition, most new spinal cord lesions cause specific symptoms such as numbness in the hands or feet, a band-like tightening around the rib cage known as the "MS hug," or difficulty with walking or going to the bathroom. If these symptoms occur, spinal cord images may show whether new lesions and breakthrough disease are present. Without any symptoms that may be related to the spinal cord, new lesions are unlikely.
Radiologists or neurologists reading MRIs frequently comment on brain-volume loss or atrophy. Our brains change as we age. In a healthy young person, an MRI shows a brain without scars or evidence of loss of brain tissue. Just as our muscles decrease in size as we age, the brain also loses tissue over time. Brain shrinkage can be seen on MRI scans as an increase in the volume of fluid and a decrease in the brain substance.
Unfortunately, MS can accelerate this tissue loss. Black holes are associated with more atrophy. Exercise, along with taking a medication for MS to reduce new lesions on MRI and subsequent black holes, can help reduce the amount of atrophy.
MRI Results Relate to Age and Different Types of MS
Similar to fingerprints, MRIs from individuals with MS are unique. Lesion size, number, and location vary, but generally, new lesions arise more frequently in early MS. More early MRI lesions may lead to more disability later in the disease. As time passes, the immune system ages along with the brain. The older immune system attacks the brain less frequently, so fewer new lesions develop later in the MS disease course.
The three most common types of MS are:
- Relapsing MS with symptom flare-ups (relapses)
- Secondary-progressive MS (SPMS), which follows relapsing MS and has a more steady progression – with or without relapses
- Primary-progressive MS (PPMS), where individuals experience a steady worsening of symptoms from the start, usually without relapses
In relapsing forms of MS, active MRI lesions are more common. In progressive forms of MS, the MRI shows fewer new lesions and increasing atrophy. Although no specific characteristic on brain imaging determines whether an individual has relapsing or progressive disease, the presence of black holes, increased atrophy, and increased volume of lesions on an MRI make progression more likely. In primary-progressive disease, the spinal cord may be especially impacted, leading to more difficulty in mobility.
Early treatment can minimize the damage done in the early phase of MS. Because DMTs reduce the formation of new lesions, effective treatment minimizes brain changes over time. Fewer lesions lead to decreased atrophy and disability.
Areas of Function Corresponding to MRI Results
As mentioned earlier, MS can sometimes be "clinically silent," where active lesions are not causing any symptoms. However, at other times, certain lesions observed through an MRI correspond specifically to some type of dysfunction, depending on where the lesion is located. For instance, a lesion on the optic nerve may cause optic neuritis, while a lesion in the brainstem can cause vertigo and/or double vision.

T2 thoracic spinal cord image with lesions (circled)
Lesions along the spinal cord cause very specific symptoms depending on their location, but in general, these typically relate to either motor (movement) or sensory (sensation) problems. When lesions occur within the anterior (front) portion of the spinal cord, motor or movement functions are affected. Difficulty with coordination and strength with moving one's arms or walking are examples of symptoms that may occur. When lesions occur within the posterior (back) portion of the spinal cord, sensory symptoms are more likely. These might include numbness, tingling, burning, and/or loss of feeling, among other sensory issues.
How high or how low the lesions occur along the spinal cord is also an important part of the equation. For instance, the part of the spinal cord that corresponds to the arms are in the cervical spine (upper portion), and lesions occurring below where these nerves come off the spinal cord may impact the legs, feet, and other function below the arms, but will not impact the functioning of the arms or hands.
Similarly, higher up on the spinal cord, lesions in the neck can cause problems anywhere at or below the neck. If lesions occur in the posterior spinal cord of the neck, changes in sensation can occur in the arms, legs, hands, or feet. This can mean pins and needles, numbness, burning, or tingling for the patient, but can also mean a decreased ability to feel the floor – resulting in decreased balance and concerns with mobility as well as the potential of falling.
Challenges to Obtaining an MRI
COST
The useful information gained from an MRI can be challenging to obtain. Cost provides one barrier to surveillance imaging. The frequency of having an MRI may be dictated by the insurance company rather than provider and consumer. Even when insurance approves an annual MRI, high co-pays may hinder access.
Ordering a brain MRI, cervical spine MRI, and thoracic spine MRI generates three separate bills and three separate co-pays or coinsurance payments. An annual MRI may recur before the last MRI bill has been fully paid. Fortunately, financial assistance can help. For those without insurance or with high co-pays, MSAA's MRI Access Fund may be able to assist. Please see the box below for more information.
MRI Funding Assistance Available
The MSAA MRI Access Fund assists with the payment of cranial (brain) and cervical-spine (upper back) magnetic resonance imaging (MRI) scans for qualified individuals who have no medical insurance or cannot afford their insurance costs. The exam must be required to help determine a diagnosis of multiple sclerosis (MS) or evaluate current MS disease progression.
For people who have already had a brain and/or c-spine MRI for their MS, MSAA will reimburse the cost of their MRI(s) up to a certain amount for qualified candidates. Under the reimbursement option, MSAA will pay the billing facility directly, as we do not reimburse individual clients. Also, please know there is a 24-month wait period to reapply for MRI assistance for new or reimbursed MRIs.
To learn more and apply, please visit the MRI Access Fund page at mymsaa.org/mri or call (800) 532-7667, ext. 154.
PHYSICAL CHALLENGES
Aside from cost, other challenges are also involved. For example, lying quietly on a metal table while images are obtained can be very difficult. Patients with back pain or spasticity can experience pain and stiffness from the hard table and the lack of motion.
In addition, most MRI tables have a weight limit of 350 pounds. Anyone heavier cannot be imaged on typical MRI machines. On occasion, body shape or size prohibits MRI even at lower weights. The tight space can be difficult to fit for some shoulders or abdomens, but more commonly causes difficulty due to claustrophobia.
A muscle relaxant can sometimes reduce the pain and stiffness associated with lying still on the table. Many people feel panic or anxiety in the closed space inside an MRI, even without having experienced claustrophobia previously. For those with anxiety during an MRI, anti-anxiety medications may help. Learning to practice deep breathing, relaxation techniques, or meditation may increase one's tolerance of being in a small space.
Despite their limitations, open MRIs offer an alternative for people who cannot tolerate closed MRIs. As noted earlier, other options may be available, including those with either a "wide-bore" or "short-bore" design, which can help to fit larger patients (up to 500 pounds in some cases), and can help individuals to feel less claustrophobic.
As noted in the section regarding the safety of contrast agents, another physical challenge to having an MRI with gadolinium is the possibility of being allergic to this contrast agent. However, this risk is very small. According to a large study, only about 12 people out of every 10,000 receiving gadolinium as a contrast agent have an allergic reaction.
Lastly, some individuals have trouble with the loud banging heard while undergoing an MRI. Fortunately, many MRI centers offer special headphones that allow the patient to listen to music during the procedure. Listening to music assists in blocking the banging noise, helps the patient to relax, and can also make the time seem to go by faster.
GETTING THE RESULTS
Waiting for MRI results can try anyone's patience. Time is needed for the radiologist to read the MRI and generate a report, then more time to communicate the results to the ordering provider. Speaking with the physician who ordered the MRI is the best way to learn of one's test results, however, the physician may not be immediately available. In the interim, some patients access results directly online or discuss results by phone with someone at the provider's office.
Unfortunately, radiology reports use terminology such as "black holes" or "T2-lesion volume," which can be difficult to interpret or cause unnecessary worry. Individuals should try to remember that extremely concerning findings on an MRI will usually lead to a direct phone call about results or may lead to an urgent appointment. Concerning findings are those that might indicate more rapid or more serious progression of the disease. More routine findings, or those that do not indicate any serious changes, can usually wait until the next appointment or be discussed with staff at the provider's office. The ordering physician is the one to best determine whether results are concerning or routine.
Whether the results are received over the phone or online – writing down questions about the MRI report or any other specific questions about the MRI itself – ensure these are addressed at the next office visit. Once this visit has been scheduled, opportunities are available to review the scan with one's provider at his or her medical office, allowing the time needed to ask these questions and address any concerns.
Most imaging locations will provide a CD with stored MRI images on request. These can be extremely useful to bring to any new neurologist or imaging location so older images can be compared to newer images. This is particularly helpful when someone with MS moves to a new location, changes providers, or switches insurance … and ends up seeing a new provider or has imaging at a different location. Maintaining a library of old images on CD can provide a comparison to the next MRI, which will ultimately be helpful to the treating physicians.
For information on the value, development, and future of imaging technology in MS, please see MSAA's interview with Dr. Rohit Bakshi.
Concluding Thoughts
While challenges exist with the cost and inconvenience of getting MRI monitoring for individuals with MS, this technology provides enormous benefits. Clear images of changes in the brain and spinal cord – without any need for radiation or invasive procedures – offer the opportunity to see whether an MS medication is working effectively. MRI images can help determine whether new symptoms reflect new disease activity or if they may have some other explanation.
In multiple sclerosis, because so many lesions do not cause specific symptoms, just feeling good is not enough. The MRI must also be free of new lesions, demonstrating that silent lesions are not occurring. Obtaining this information can provide reassurance that treatment has been effective or evidence that a change needs to be made.
Research into new techniques with MRI may increase the value of MRI in the future. Some imaging facilities now provide a specific quantification of the total-lesion volume and the extent of atrophy of the brain.
When images are compared over time, atrophy can be specifically measured and may indicate worsening disease even without any new lesions. Newer techniques may show disease activity in gray matter more effectively and illustrate information about pathology not well seen on conventional MRI. As these research techniques enter mainstream clinical medicine, MRI may have even more value in the future.
For the present, MRI allows for a window into the brain and spinal cord, with a clear view of disease progression, new inflammation, and treatment effect. This window into multiple sclerosis can help optimize treatment and help make effective disease-management decisions to limit the impact of multiple sclerosis.
ABOUT THE AUTHOR
 Author Dr. Jill Conway is a neurologist who currently serves as Director of the MS Center at Atrium Healthcare in Charlotte, North Carolina. She earned her medical degree from the University of Illinois and completed her neurology residency at the University of Pennsylvania. Dr. Conway completed a two-year multiple sclerosis fellowship, with a clinical research focus, at the University of Pennsylvania. This fellowship training was sponsored by the National Multiple Sclerosis Society. Dr. Conway has a longstanding interest in clinical ethics and clinical research ethics, and has served on Carolinas Medical Center's Ethics Committee. Her research interests include cognitive function in multiple sclerosis, treatment of mood disorders in MS, new and emerging therapies, neuromyelitis optica, and issues related to women and multiple sclerosis.
Author Dr. Jill Conway is a neurologist who currently serves as Director of the MS Center at Atrium Healthcare in Charlotte, North Carolina. She earned her medical degree from the University of Illinois and completed her neurology residency at the University of Pennsylvania. Dr. Conway completed a two-year multiple sclerosis fellowship, with a clinical research focus, at the University of Pennsylvania. This fellowship training was sponsored by the National Multiple Sclerosis Society. Dr. Conway has a longstanding interest in clinical ethics and clinical research ethics, and has served on Carolinas Medical Center's Ethics Committee. Her research interests include cognitive function in multiple sclerosis, treatment of mood disorders in MS, new and emerging therapies, neuromyelitis optica, and issues related to women and multiple sclerosis.
Back
Cervical Mri Bright Spot at Back of Skull
Source: https://mymsaa.org/publications/motivator/summer-fall18/cover-story/
0 Response to "Cervical Mri Bright Spot at Back of Skull"
Post a Comment